AEGIS: AI-Guided X-ray Radiation Reduction
AI Meets Radiation Safety
Our AEGIS solution is helping to protect the health and safety of medical staff and patients during fluoroscopy-guided procedures across the United States. Our system uses Artificial Intelligence (AI), an electromechanical shutter, and advanced image processing to selectively block unnecessary radiation during fluoroscopy imaging. In partnership with Omega Medical Imaging, AEGIS is now used in dozens of US hospitals.

Guided by AI, our electromechanical shutter blocks out unnecessary radiation, protecting the safety of medical staff and patients

Radiation Risks in Fluoroscopy
Minimally invasive procedures are the way of the future as they eliminate surgery and enable shorter procedures and quicker recoveries. These procedures are guided by fluoroscopy: a medical imaging technique that uses a series of X-rays to obtain real time moving images of the internal structures of a patient’s body.
The number of X-rays required for fluoroscopy exposes both medical staff and patients to high levels of ionizing radiation, which has been shown to increase the risk of cancer,1, 2 stroke,3 cataracts,4 and other conditions.

Hands-Free Radiation Reduction by Over 60%
AEGIS stands apart from other technologies that simply filter radiation. With ultrafast collimation and an automatically identified Region of Interest (ROI), we completely block unnecessary radiation, allowing for hands-free radiation reduction and an unchanged workflow for medical staff. AEGIS has been shown to reduce radiation by over 60%.

Uncompromised Image Quality
Our advanced image processing technology maintains the high-quality images that physicians demand. Our system opens the shutter to the full field of view only once per second, limiting radiation to the areas where visualization is needed for the remaining frames. The result is a seamless integration of the ROI with the full field of view, providing uncompromised image quality.
Procedure-Specific AI Tracking
Our AI tracks the physician’s ROI by detecting the movements of key items such as contrast fluid, catheters, and endoscopes. The ROI then automatically controls the shutter movements to collimate areas of less interest, reducing unnecessary radiation.
Trained for gastrointestinal endoscopic retrograde cholangiopancreatography (GI ERCP) and cardiac procedures, our specialized AI can be adapted for any fluoroscopy procedure. Contact us to learn more about integrating AEGIS with your fluoroscopy system.
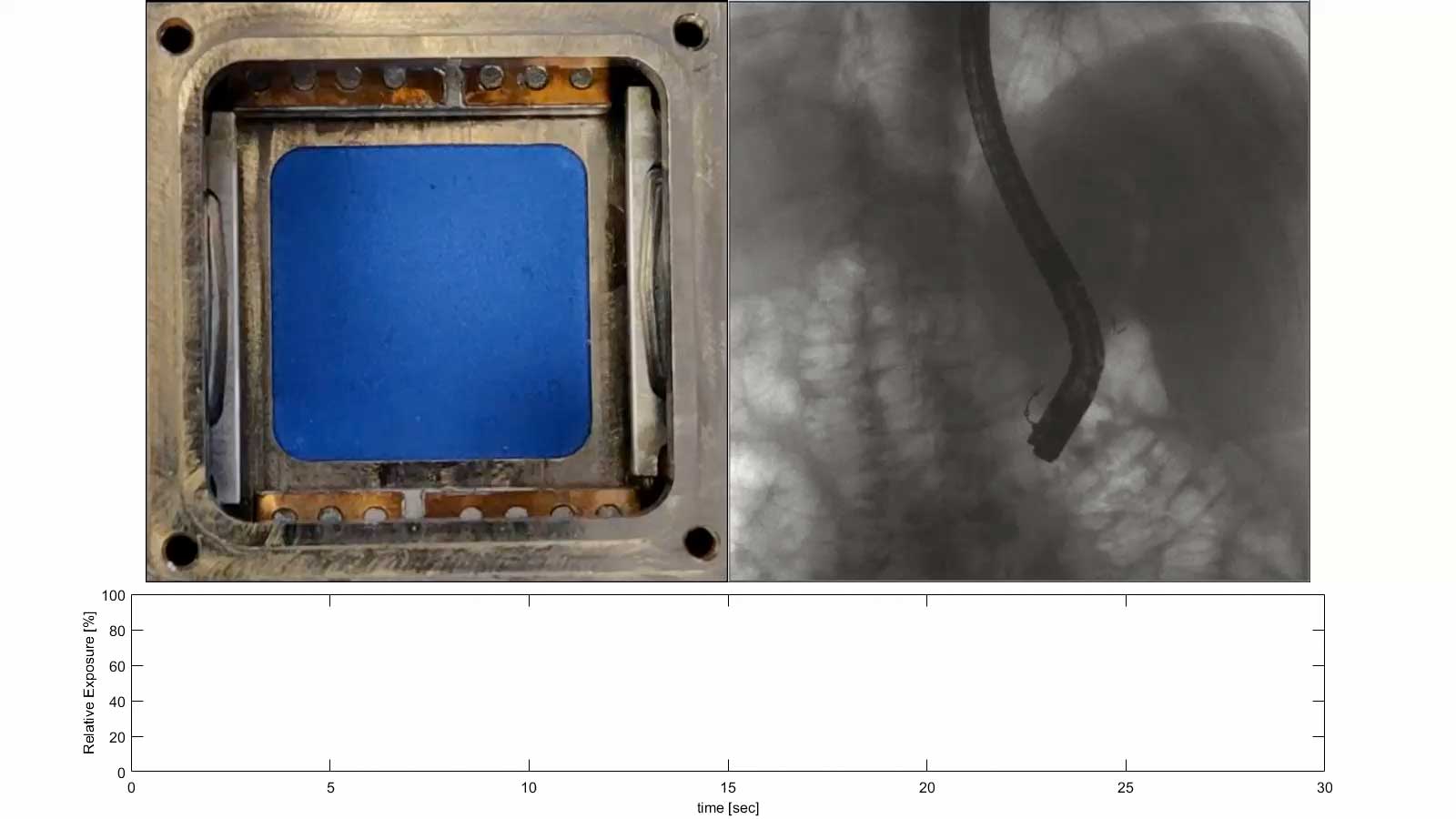
Left: The shutter, with 4 lead blades, placed on top of the X-ray source.
Right: The full image as seen by the physician. The white frame is the ROI and corresponds to the open area in the shutter.
Bottom: The radiation level compared to a fully open shutter.
Ongoing Development
As we expand the use of AEGIS and broaden our reach we are continuously improving the tracking performance and training our AI system on new procedures. We are proud to be part of the local tech community and to be doing all of our development work, as well as manufacturing, integration, and testing, in our Vancouver office.




Related Publications
Automatic detection and tracking of the region of interest during fluoroscopy-guided procedures for radiation exposure reduction
Date: February 15, 2021 | View Publication
Abstract
The rise in number of fluoroscopy-guided procedures has prompted strategies for radiation management in order to minimize exposure to ionizing radiation in patients and healthcare personnel. The FluoroShield system utilizes an artificial intelligence (AI) approach towards radiation exposure reduction. The system automatically tracks the region of interest (ROI) in real-time, controls a rapid lead shutter for collimating the X-ray beam to the ROI, and blends the imaged ROI with the entire field of view that is updated at a lower frame rate to present, at all times, a full image to the operator. In this work, we discuss the AI-based component of the system that is used for tracking the ROI in endoscopic procedures. Known as the auto-ROI processor (ARP), the methodology comprises a merged architecture of convolutional neural networks for object detection that allows for both fine and contextual features to be captured. The detection probabilities are incorporated within a particle filtering framework for spatial and temporal updating of the ROI in a Bayesian approach. The ARP’s performance is evaluated on fluoroscopic sequences, taking into consideration the estimated radiation reduction rates. The reduction in radiation exposure based on simulations is comparable to the reported values in a clinical study.
Poster: An AI Enabled Dynamic Coning System Reduces Radiation Dose During Fluoroscopy
Date: November 20, 2019 | Download: AHA Poster November 2019 (PDF)
Reducing the size of the radiated field (“coning”) significantly decreases the radiation dose to both patient and medical staff during fluoroscopic procedures. Even with excellent coning, the physician’s attention is typically focused on a small part of the monitor image, e.g. where there is movement of a catheter. The remainder of the irradiated field is essential for orientation.
Sources
- Rajaraman P, Doody MM, Yu CL, et al. Journal Club: Cancer Risks in U.S. radiologic technologists working with fluoroscopically guided interventional procedures, 1994-2008. American Journal of Roentgenology. 2016;206(5):1101-1109. doi:10.2214/ajr.15.15265
- Stahl CM, Meisinger QC, Andre MP, Kinney TB, Newton IG. Radiation risk to the fluoroscopy operator and staff. American Journal of Roentgenology. 2016;207(4):737-744. doi:10.2214/ajr.16.16555
- Rajaraman P, Doody MM, Yu CL, et al. Incidence and mortality risks for circulatory diseases in US radiologic technologists who worked with fluoroscopically guided interventional procedures, 1994–2008. Occupational and Environmental Medicine. 2015;73(1):21-27. doi:10.1136/oemed-2015-102888
- Vano E, Kleiman NJ, Duran A, Romano-Miller M, Rehani MM. Radiation-associated lens opacities in catheterization personnel: Results of a survey and direct assessments. Journal of Vascular and Interventional Radiology. 2013;24(2):197-204. doi:10.1016/j.jvir.2012.10.016

