ATMOS: Noninvasive Treatment for Emphysema
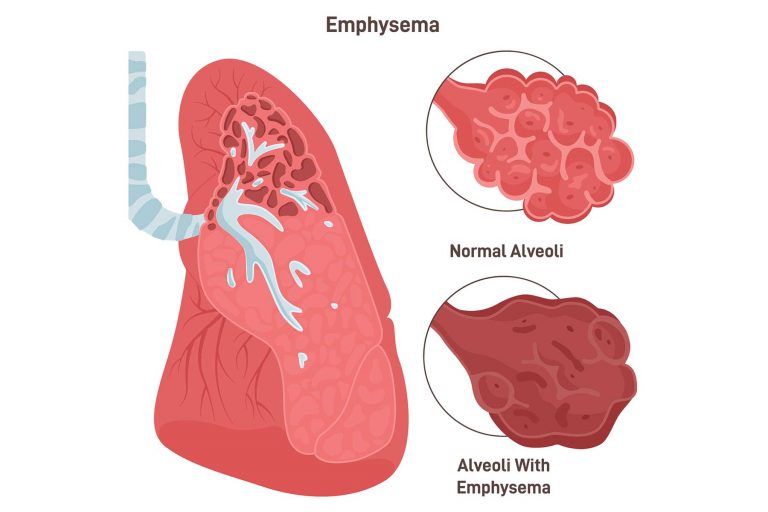
What is Emphysema?
Emphysema is a type of chronic obstructive pulmonary disease (COPD) that causes the progressive and irreversible destruction of lung tissue, leading to breathlessness and decreased lung function. This debilitating disease results in reduced ability to exercise or perform daily tasks, and overall worsening quality of life.
Emphysema is most often caused by prolonged tobacco smoking, but can also result from genetic conditions or exposure to air pollution. Currently, there is no cure for this disease that affects millions of people globally, with COPD being the third leading cause of death worldwide.1

Noninvasive Treatment
Invasive lung volume reduction surgery and experimental bronchoscopic treatments often carry a high risk of complications, making them unsuitable for many patients.2 Our noninvasive ATMOS device will be able to treat a wider range of patients without the complications of invasive procedures, improving millions of lives globally.
The ATMOS Solution
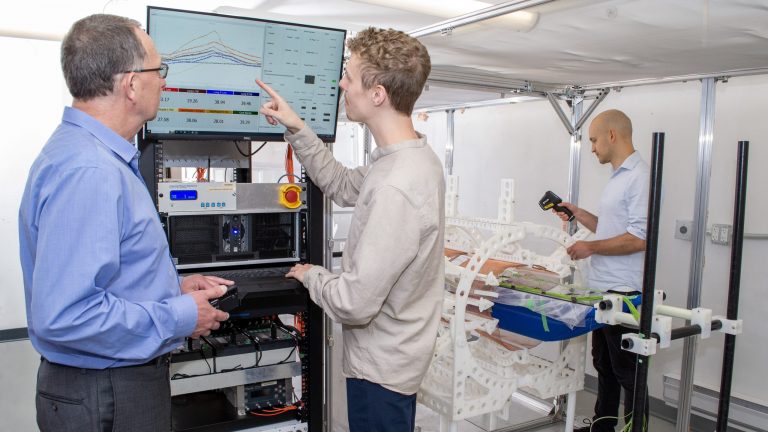
At IKOMED we are developing an innovative, noninvasive treatment that applies radiofrequency (RF) energy to target diseased tissue and improve breathing in patients. Our goal is to slow the progression of emphysema while improving the lung function, comfort, health, and life expectancy of COPD patients.

How it Works
Our noninvasive treatment heats diseased tissue leading to tissue remodeling, resulting in the shrinking of diseased areas allowing the lungs to function better. In early preclinical testing, our treatment led to improved breathing mechanics and exercise capability. Currently our device is undergoing additional in vivo testing on the path to clinical studies.
Related Publications
Development of a unilateral porcine emphysema model induced by porcine pancreatic elastase
Date: September 28, 2023 | View Publication
Abstract
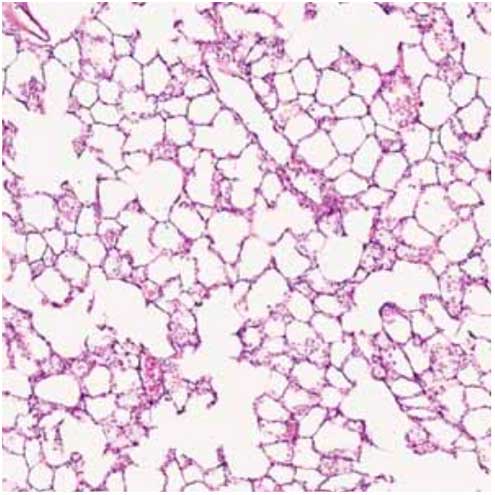
Emphysema is one of the pathological hallmarks of chronic obstructive pulmonary disease. We have recently reported that radiofrequency therapy improves lung function in rodent models of emphysema. However, preclinical data using large animals is necessary for clinical translation. Here, we describe the work performed to establish a unilateral porcine emphysema model. Different doses of porcine pancreatic elastase (PPE) were instilled into the left lung of 10 Yucatan pigs. Three additional pigs were used as controls. Six weeks after instillation, lungs were harvested. Lung compliance was measured by a water displacement method and plethysmography. Systematic uniform random sampling of the left and right lungs was performed independently to measure alveolar surface area using micro-computed tomography (micro-CT) and histology. In pigs instilled with 725– 750 U/kg of PPE (PPE group, n = 6), the compliance of the left lung was significantly higher by 37.6% than that of the right lung (P = 0.03) using the water displacement method. With plethysmography, the volume of the left lung was significantly larger than that of the right lung at 3, 5, and 10 cmH2O. Measurements from either micro-CT or histology images showed a significant decrease in alveolar surface area by 14.2% or 14.5% (P = 0.031) in the left lung compared with the right lung of the PPE group. A unilateral model for mild emphysema in Yucatan pigs has been established, which can now be used for evaluating novel therapeutics and interventional strategies.
Radiofrequency therapy improves exercise capacity of mice with emphysema
Date: October 8, 2021 | View Publication
Abstract
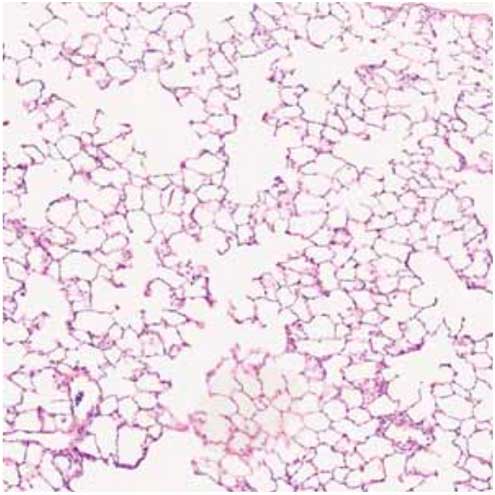
Emphysema is a common phenotype of chronic obstructive pulmonary disease (COPD). Although resection of emphysematous tissue can improve lung mechanics, it is invasive and fraught with adverse effects. Meanwhile, radiofrequency (RF) treatment is an extracorporeal method that leads to tissue destruction and remodeling, resulting in “volume reduction” and overall improvement in lung compliance of emphysematous lungs. Whether these changes lead to improved exercise tolerance is unknown. Here, we investigated the effectiveness of RF treatment to improve the exercise capacity of mice with emphysema. Fifty-two mice (7 weeks of age) were used in this experiment. A bilateral emphysema model was created by intratracheally instilling porcine pancreatic elastase (PPE) (1.5U/100 g body weight). RF treatment (0.5 W/ g body weight) was administered extracorporeally 14 days later and mice were sacrificed after another 21 days. The exercise capacity of mice was measured using a treadmill. Treadmill runs were performed just before PPE instillation (baseline), before RF treatment and before sacrifice. Following sacrifice, lung compliance and mean linear intercept (Lm) were measured and fibrosis was assessed using a modified Ashcroft score. There were 3 experimental groups: controls (instilled with saline, n = 12), emphysema (instilled with porcine pancreatic elastase, PPE, n = 11) and emphysema + treatment (instilled with PPE and given RF, n = 9). At endpoint, the maximum velocity of the emphysema + treatment group was significantly higher than that of the emphysema group, indicating improved exercise tolerance (86.29% of baseline vs 61.69% of baseline, p = 0.01). Histological analysis revealed a significant reduction in emphysema as denoted by Lm between the two groups (median 29.60 µm vs 35.68 µm, p = 0.03). The emphysema + treatment group also demonstrated a higher prevalence of lung fibrosis (≧Grade 3) compared with the emphysema group (11.7% vs 5.4%, p < 0.01). No severe adverse events from RF were observed. RF treatment improved the exercise capacity of mice with emphysema. These data highlight the therapeutic potential of RF treatment in improving the functional status of patients with COPD.
Chronic Obstructive Pulmonary Disease (COPD) is a common inflammatory disorder of the lung, characterized by persistent airflow limitation. In COPD, the airways become progressively narrowed, resulting in impaired lung function, increased work of breathing, and shortness of breath. Currently, COPD affects over 300 million people worldwide and is the leading cause of hospitalizations in many industrialized countries such as the United States (US) and Canada. COPD is responsible for over 4.5 million deaths annually and is one of the major causes of mortality worldwide1,2. Typically, smoking-related COPD is accompanied by emphysema, which is characterized by the destruction of lung tissue resulting in the loss of alveolar integrity, enlargement of the alveolar spaces, poor gas exchange, and airway collapse due to the loss of elastic recoil3. This remodeling results in impairment in airflow and hypoxemia.
Lung volume reduction surgery (LVRS) is a potential treatment for COPD, but it is limited to a subpopulation of patients with severe emphysema involving the upper lobes and with low exercise capacity. LVRS has been demonstrated to reduce breathlessness, improve exercise capacity and lung function, and prolong survival4,5. The physiologic basis for this treatment is that by selectively removing the most diseased segments of the lung, the lung deflates and there is better matching of ventilation and (blood) perfusion, leading to less gas trapping and improved gas exchange, respectively, during exercise6. However, LVRS is invasive and fraught with considerable perioperative morbidity and mortality related to the procedure. As such, very few sites currently perform LVRS2,3,7. To overcome the high invasiveness and the cost of LVRS, endoscopic lung volume reduction (ELVR) including bronchoscopic lung volume reduction (BLVR) has been developed using one-way valves, coil implants (LVR coil, LVR-C), sealants/hydrogels (BioLVR), airway bypass stents, and bronchial thermal vapor ablation (BTVA) therapy. However, these methods are still invasive and expensive and fraught with certain adverse effects including hemoptysis and pneumothorax8,9,10,11,12. According to a multicenter randomized controlled trial to evaluate endobronchial valves (EBV), 26.6% (34/128) of EBV subjects developed pneumothorax and four deaths occurred (4/128)8. Moreover, it is still difficult to determine the patients who benefit from ELVR9,10.Thus, minimally-invasive (or ideally completely non-invasive) modalities to deliver the benefits of LVRS are still clinically needed.
Radiofrequency (RF) is commonly used to treat solid tumors and atrial fibrillation in a procedure called RF ablation (RFA)12,13. The principle of RFA is that RF waves agitate water molecules in the surrounding tissue, producing friction and heat, which in turn induce cellular death via coagulation and necrosis12. Healthy regions with good blood supply are relatively spared from thermal damage because the circulating blood can absorb the external heat and carry it away via a process known as a “heat sink effect”14. A well-known pathologic feature of emphysema is pulmonary vascular remodeling, which causes diminution of blood flow to the emphysematous regions15, making these areas susceptible to thermal injury. Based on these concepts, we applied RF therapy extracorporeally to destroy emphysematous regions of the COPD lung in a rodent model of emphysema. Previously, we showed that the application, using external electrodes, of RF energy in the form of electromagnetic waves improved lung compliance by selectively heating pulmonary emphysematous tissue and inducing mild fibrosis in the affected lung while sparing normal lung regions16. However, in that study, we did not determine whether the physiological changes led to improvements in the functional status of animals with emphysema which would a critical indicator of a beneficial therapeutic effect. Here, we investigated the effectiveness of extracorporeal RF treatment in improving the exercise capacity of mice with emphysema.
External radiofrequency as a novel extracorporeal therapy for emphysema
Date: November 1, 2020 | View Publication
Abstract
COPD is characterised by the destruction of lung tissue resulting in alveolar tissue destruction, enlargement of alveolar spaces, poor gas exchange and airway collapse due to the loss of elastic recoil. Lung volume reduction surgery is effective in reducing long-term morbidity and mortality of patients with severe emphysema who have a predominance of upper lobe disease and are able to tolerate the surgical procedure. However, the financial cost and the perioperative morbidity and mortality of the procedure have limited its application in clinical practice. Here, we investigated the possibility of using external radiofrequency (RF) as a novel extracorporeal treatment for emphysema in a rat model of unilateral emphysema.
Sources
- Chronic obstructive pulmonary disease (COPD). World Health Organization. Updated March 16, 2023. Accessed May 9, 2023. https://www.who.int/news-room/fact-sheets/detail/chronic-obstructive-pulmonary-disease-(copd)
- National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl Med. 2003;348(21):2059-73. doi: 10.1056/NEJMoa030287

